How we realize an ocular prosthesis
Before describing stages of an ocular prosthesis construction, we remind you that our purpose is not only the coverage or replacement of the eye but also to improve prosthesis motility, preserving eyelid functionality and restoration of an adequate psychological condition after trauma.
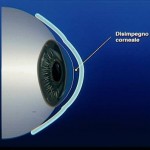
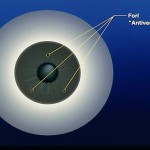
The prosthetic application is designed to achieve these results over time, counteracting the loss of tissue elasticity due to aging. Acrylic resin (PMMA) can adapt and change the prosthesis shape for several times and without limitations except those due to the injury suffered. The objectives of the prosthetic application are:
- Maintenance of the anophthalmic socket volume
- Reduction of the enophthalmos (upper tarsal sulcus)
- Restoration of the excursion and eyelid movements